Nanofiber-Based Drug Delivery System for Diabetic Foot Ulcers (DFU): A Comprehensive Review
 DOI:
DOI:
https://doi.org/10.33974/65hmzn18
Keywords:
Nanofibers, Drug Delivery Systems, Diabetic Foot Ulcers, Wound Healing, Tissue EngineeringAbstract
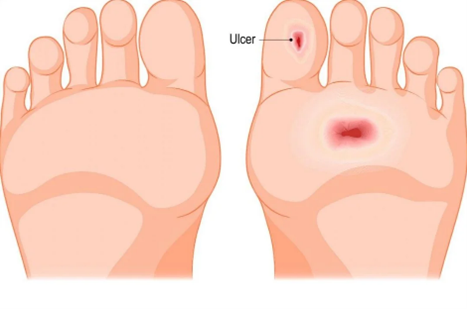
Diabetic foot ulcers (DFUs) are a major complication of diabetes, contributing to high morbidity, decreased quality of life, and even limb amputation. Traditional treatments, such as wound dressings and systemic therapies, often fail to sufficiently promote healing or prevent recurrence, underscoring the need for novel therapeutic approaches. Nanofiber-based drug delivery systems have emerged as a promising solution, offering unique advantages like high surface area, tunable porosity, and the ability to encapsulate and deliver therapeutic agents in a controlled and sustained manner. These systems can deliver various bioactive substances, including growth factors, antibiotics, and anti-inflammatory drugs, directly to the wound site, promoting faster healing, reducing infection, and enhancing tissue regeneration. The materials used for nanofiber fabrication include natural polymers, such as collagen and chitosan, and synthetic polymers like polycaprolactone (PCL) and polylactic acid (PLA), which can be tailored to the specific needs of DFU treatment. Electrospinning, a versatile technique, is primarily employed to produce nanofibers with precise control over diameter and morphology, allowing for the customization of drug release profiles. This article provides a comprehensive review of the use of nanofiber-based drug delivery systems in the treatment of DFUs, focusing on their advantages, the therapeutic agents involved, materials used, and fabrication techniques. The review highlights the potential of these systems to revolutionize DFU management, offering a promising avenue for improving healing outcomes and reducing complications associated with diabetic foot ulcers.
Downloads
References
Yazdanpanah, L., Nasiri, M., & Adarvishi, S. (2015). Literature review on the management of diabetic foot ulcer. World Journal of Diabetes, 6(1), 37. https://doi.org/10.4239/wjd.v6.i1.37
Kamal, R., Razzaq, A., Khan, Z. U., Khan, N. U., Menaa, F., Iqbal, H., & Cui, J. (2022). Evaluation of cephalexin-loaded PHBV nanofibers for MRSA-infected diabetic foot ulcers treatment. Journal of Drug Delivery Science and Technology, 71, 103349. https://doi.org/10.1016/j.jddst.2022.103349
Mariam, T. G., Alemayehu, A., Tesfaye, E., Mequannt, W., Temesgen, K., Yetwale, F., & Li-menih, M. A. (2017). Prevalence of diabetic foot ulcer and associated factors among adult diabetic patients who attend the diabetic follow-up clinic at the University of Gondar Referral Hospital, North West Ethiopia, 2016: Institutional-based cross-sectional study. Journal of Diabetes Re-search, 2017, 2879249. https://doi.org/10.1155/2017/2879249
Raja, J. M., Maturana, M. A., Kayali, S., Khouzam, A., & Efeovbokhan, N. (2023). Diabetic foot ulcer: A comprehensive review of pathophysiology and management modalities. World Journal of Clini-cal Cases, 11(8), 1684. https://doi.org/10.12998/wjcc.v11.i8.1684
Awasthi, A., Gulati, M., Kumar, B., Kaur, J., Vish-was, S., Khursheed, R., Porwal, O., Alam, A., Kr, A., Corrie, L., & Kumar, R. (2022). Recent progress in development of dressings used for diabetic wounds with special emphasis on scaffolds. Bi-oMed Research International, 2022, 1659338. https://doi.org/10.1155/2022/1659338
Kamble, P., Sadarani, B., Majumdar, A., & Bhullar, S. (2017). Nanofiber based drug delivery systems for skin: A promising therapeutic approach. Jour-nal of Drug Delivery Science and Technology, 41, 124-133. https://doi.org/10.1016/j.jddst.2017.06.007
Jain, R., Shetty, S., & Yadav, K. S. (2020). Unfold-ing the electrospinning potential of biopolymers for preparation of nanofibers. Journal of Drug De-livery Science and Technology, 57, 101604. https://doi.org/10.1016/j.jddst.2020.101604
Subbiah, T., Bhat, G. S., Tock, R. W., Parameswa-ran, S., & Ramkumar, S. S. (2005). Electrospin-ning of nanofibers. Journal of Applied Polymer Science, 96(2), 557-569. https://doi.org/10.1002/app.21527
Kamble, P., Sadarani, B., Majumdar, A., & Bhullar, S. (2017). Nanofiber based drug delivery systems for skin: A promising therapeutic approach. Jour-nal of Drug Delivery Science and Technology, 41, 124-133. https://doi.org/10.1016/j.jddst.2017.06.007
Liu, Y., Zhou, S., Gao, Y., & Zhai, Y. (2019). Elec-trospun nanofibers as a wound dressing for treat-ing diabetic foot ulcer. Asian Journal of Pharma-ceutical Sciences, 14(2), 130-143. https://doi.org/10.1016/j.ajps.2018.08.005
Chiu, A., Sharma, D., & Zhao, F. (2021). Tissue engineering-based strategies for diabetic foot ul-cer management. Advances in Wound Care, 12(3), 145-167. https://doi.org/10.1089/wound.2021.1217
Xu, X., Wang, X., Qin, C., Khan, A. U. R., Zhang, W., & Mo, X. (2021). Silk fibroin/poly-(L-lactide-co-caprolactone) nanofiber scaffolds loaded with Huangbai Liniment to accelerate diabetic wound healing. Colloids and Surfaces B: Biointerfaces, 199, 111557. https://doi.org/10.1016/j.colsurfb.2020.111557
Cam, M. E., Yildiz, S., Alenezi, H., et al. (2020). Evaluation of burst release and sustained release of pioglitazone-loaded fibrous mats on diabetic wound healing: An in vitro and in vivo compari-son study. Journal of the Royal Society Interface, 17(162), 20190712. https://doi.org/10.1098/rsif.2019.0712
Almukainzi, M., El-Masry, T. A., Negm, W. A., et al. (2022). Co-delivery of gentiopicroside and thymoquinone using electrospun m-PEG/PVP nanofibers: In-vitro and in vivo studies for anti-bacterial wound dressing in diabetic rats. Interna-tional Journal of Pharmaceutics, 625, 122106. https://doi.org/10.1016/j.ijpharm.2022.122106
Davani, F., Alishahi, M., Sabzi, M., Khorram, M., Arastehfar, A., Zomorodian, K. (2021). Dual drug delivery of vancomycin and imipenem/cilastatin by coaxial nanofibers for treatment of diabetic foot ulcer infections. Materials Science and Engi-neering: C, 123, 111975. https://doi.org/10.1016/j.msec.2021.111975
Alzahrani, D. A., Alsulami, K. A., Alsulaihem, F. M., Bakr, A. A., Booq, R. Y., Alfahad, A. J., Aodah, A. H., Alsudir, S. A., Fathaddin, A. A., Alyamani, E. J., & Almomen, A. A. (2024). Dual drug-loaded coaxial nanofiber dressings for the treatment of diabetic foot ulcer. International Journal of Na-nomedicine, 19, 5681-5703. https://doi.org/10.2147/IJN.S377719
Kamal, R., Razzaq, A., Khan, Z. U., Khan, N. U., Menaa, F., Iqbal, H., & Cui, J. (2022). Evaluation of cephalexin-loaded PHBV nanofibers for MRSA-infected diabetic foot ulcers treatment. Journal of Drug Delivery Science and Technology, 71, 103349. https://doi.org/10.1016/j.jddst.2022.103349
Zhu, Y., Zhou, W., Xiang, J., Wu, M., Chen, Z., Yang, Z., Wei, R., & Cai, L. (2023). Deferoxamine-loaded Janus electrospun nanofiber dressing with spa-tially designed structure for diabetic wound heal-ing. Materials & Design, 233, 112166. https://doi.org/10.1016/j.matdes.2023.112166
Anand, S., Pandey, P., Begum, M. Y., Chidam-baram, K., Arya, D. K., Gupta, R. K., Sankhwar, R., Jaiswal, S., Thakur, S., Rajinikanth, P. S. (2022). Electrospun biomimetic multifunctional nano-fibers loaded with ferulic acid for enhanced an-timicrobial and wound-healing activities in STZ-Induced diabetic rats. Pharmaceuticals, 15(3), 302. https://doi.org/10.3390/ph15030302
Jeckson, T. A., Neo, Y. P., Sisinthy, S. P., Foo, J. B., Choudhury, H., & Gorain, B. (2021). Formulation and characterisation of deferoxamine nanofiber as potential wound dressing for the treatment of diabetic foot ulcer. Journal of Drug Delivery Sci-ence and Technology, 66, 102751. https://doi.org/10.1016/j.jddst.2021.102751
Published
Issue
Section
Categories
License
Copyright (c) 2026 S. Gajalakshmi, A. Jayakumar (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
License Terms
This is an open-access article published in the International Journal of Research in Pharmaceutical Sciences and Technology (IJRPST) by Rubatosis Publications.
It is distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0), which permits unrestricted use, distribution, reproduction, and adaptation in any medium or format, provided the original author(s) and source are appropriately credited, a link to the license is provided, and any changes made are indicated.
To view a copy of this license, visit: https://creativecommons.org/licenses/by/4.0/
For any further queries or permissions beyond the scope of this license, please contact: editor@rubatosis.org




